First questions
-
01¿What is lactose?
-
02What is lactase?
Lactase is the last enzyme to appear and mature in the baby that is about to be born. It shows maximum activity at the time of birth and during the breastfeeding phase and starts to decline after weaning. It is the disaccharidase necessary for digestion and unfolding of lactose into two simple sugars, glucose and galactose.

-
03Where is lactase found?
Lactase is found in the small intestine and its distribution is irregular. Its activity is maximum if the first portions of the jejunum and non-existent in the stomach and the colon.

-
04What direct intestinal symptoms does LI cause?
The symptoms are frequently presented after ingestion of dairy products and can be:
· Abdominal pain (100%)
· Abdominal distension (100%)
· Bowel sounds (100%)
· Flatulence (100%)
· Nausea (78%)
· Vomiting (78%)
· Diarrhoea (70%)
· Constipation (30%)
-
05Do all people have the same symptoms?
The variability of the symptoms and their intensity will depend on various factors for each individual.
Consumption factor
· Quantity of lactose ingested.
· Type of dairy ingested (milk, yoghurt, etc.)
· Simultaneous consumption with other food.Individual/physiological factor
· Level of individual lactase activity.
· Speed of gastric emptying.
· Intestinal motility (visceral hypersensitivity)
· Individual’s particular macrobiota (colon)
· Colon’s capacity for water absorption.Probably the two most important factors for determining the presence of factors are: the quantity of lactose ingested and the colon’s capacity for water absorption in the compensation and rescue of carbohydrates, re-absorbing water and fatty acids from the short chain.
-
06What other unspecific symptoms may occur?
In some individuals there may be a series of symptoms called systemic symptoms (beyond the intestinal area) due to the production of toxic metabolites such as acetaldehyde, ethanol, peptides, etc.:· Headache.
· Fatigue.
· Muscle and joint pain.
· Skin problems
· Dry mucous membranes.
· Anxiety
· Mouth ulcers.
· Dejection and depression.
· Allergic reactions.
· Lack of concentration. -
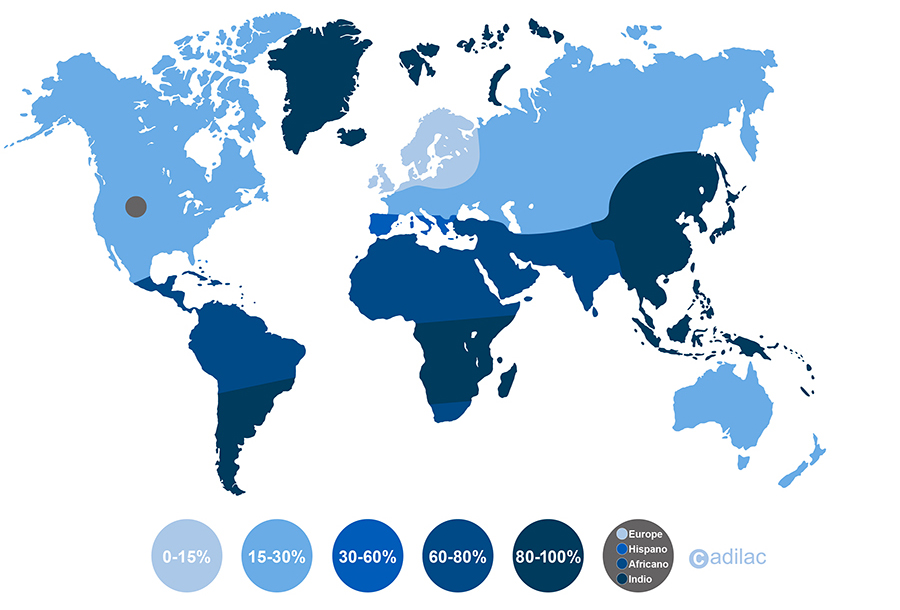
07Which races are most affected?
70% of the adult global population has primary lactase deficiency, except for towns in the north of Europe. Centuries ago, these towns, far from the sea, with little access to sunlight, severe climates and difficulties for agriculture, found in dairy consumption a means of survival and became “farmers”. This fact provoked a genetic mutation that allowed them not to stop producing lactase and to be lactose-persistent.
-
08What types of lactase deficiency exist?
1. Acquired hypolactasia or primary lactase deficiency (LNP Lactase-nonpersistence)
GENETIC CAUSE, PROGRESSIVE, NO RECOVERY
A progressive loss of lactase production occurs, and therefore a gradual loss of the ability to digest lactose. It usually occurs throughout life in certain ethnic groups and has a genetic cause. People with this intolerance are noticing how milk intake causes more and more symptoms. More than 70% of the world population suffers from this deficiency. When it is of a primary / genetic nature, there is no possible cure because the individual does not recover the enzyme and the symptoms are only alleviated with the suspension of dairy products in the diet. Lactose intolerance is not dangerous and is very common in adults.
2. Hypolactasia or secondary lactase deficiency
OTHER CAUSE, TEMPORARY, RECOVERABLEThe reduced production of lactase is secondary, as it is caused by another motive or enteropathy. Once the person is cured and when the intestinal mucosa has regenerated, the poor digestion disappears.
Possible causes:
· Premature babies present a congenital lactase deficiency because the lactase is mainly developed in the third trimester of pregnancy. The baby is born with lower lactase activity than that needed and presents problems of poor digestion of the maternal colostrum. This is a transitory situation, with few symptoms, which corrects itself spontaneously.
· Bacterial infectious gastroenterocolitis.
· Viral infectious gastroenterocolitis.
· Parasite infectious gastroenterocolitis.
· Coeliac illness.
· Crohn’s disease.
· Malnutrition due to prolonged diarrhoea.
· Malnutrition due to anorexia or bulimia.
· Short intestine syndrome.
· Irritable intestine syndrome.
· Taking certain antibiotics
· Excess bacterial growth.3. Alactasia or congenital lactase deficiency
(CLD Congenital lactase deficiency)
GENETIC, FROM BIRTH, NO RECOVERYThis is an unusual form of deficiency, where the newborn presents symptoms with the first exposure to maternal milk. It is caused by a genetic defect caused by autosomal recessive mutation of the LCT gene that codes the lactase, causing null or minimum enzyme activity. Very few cases have been detected in the world (40), with the majority being in Finland (16). It is essential to prescribe a lactose-free diet for the nursing infant in order to avoid injury and serious complications in their development.
-
09Can lactose intolerance be considered a recent occurrence?
No.
No. The genetic analysis of remains from the first populations that began to settle and farm, in the Neolithic era (8000 BC) suffered from primary lactase deficiency or LNP.
Hippocrates, considered to be the father of modern dietetics and medicine, described back in 400 BC a series of intestinal symptoms in some people after consuming dairy products such as milk and cheese.
However, it was in 1950, when the consumption of dairy was becoming generalised on a global scale, that the first documented medical cases of lactose intolerance appeared.
-
10Are lactose digestion problems the same for everyone?
No. In this primary deficiency of lactase, no two people are the same. As we explain in greater detail in the section What is LI? each person has their own threshold of sensitivity and although we are all people with poor digestion of lactose, there are people who can digest certain quantities of lactose without symptoms (up to 12g in a single dose accompanied by other food), and others than with less than 6g present symptoms of lactose intolerance.
-
11Why is it important to detect and treat it quickly?
Lactase is one of the most delicate and vulnerable intestinal enzymes. If we continue to ingest lactose, the injury to the intestinal mucosa will grow and a vicious cycle will begin: Injury to mucosa/poor digestion of lactose which will be increasingly difficult to resolve.
-
12Is lactose intolerance different to allergy to cow’s milk protein or CMP?
Although both ailments have the same origin (milk or dairy), they have nothing in common (allergy to CMP is a reaction of the immune system to milk protein). This explains why on the market you can find products that are suitable for the lactose intolerant (lactose-free milk, cheese, etc.) that are not suitable for those allergic to CMP.

-
13How to live with intolerance?
The lack of milk in the diet can cause significant mineral needs (calcium, phosphorous, potassium, magnesium, zinc and iron), fat-soluble vitamins (A, D, E, K) and water-soluble (B1, B2, B6, B9, B12 and C). The most common complications can be loss of weight and malnutrition. Therefore, it is essential to consume other products rich in these substances, which fortunately are easy to find.
Alternative mineral sources:
· Calcium: Fish, spinach, almonds.
· Phosphorous: Walnuts, sardines, eggs.
· Potassium: Bananas, chicken, avocado.
· Magnesium: Nuts, beans.
Alternative vitamin sources:
· A: Carrots, pulses.
· D: Organism through sunshine, cod liver.
· E: Vegetable oils, nuts.
· K: Tomato, celery, blackberry. -
14Are fermented dairy products better tolerated?
Fermented dairy products, such as mature/semi-mature cheeses, yoghurts, fermented milks, curd, etc. are better tolerated because in the fermentation process, the lactic ferments (bacterias) hydrolyse the lactose, producing lactic acid and reducing their presence.:
-
15Why yogurt is better tolerated?
Yogurt has characteristics that make it more digestive compared to other fermented products. Although we must not forget that the final product still contains lactose (approximately 4-5g / 100g).
1. In the fermentation process, the lactic ferments (bacterias) hydrolyse the lactose, producing lactic acid and reducing their presence.
2. In the case of yoghurt, the lactic ferments (Lactobacillus bulgaricus and Streptococcus thermophilus alive in the final product) continue consuming the lactose present in the final product after being ingested, this facilitating the digestion of the lactose present in the yoghurt. (EFSA, 2011)
3. In the case of yoghurt, the lactic ferments (Lactobacillus bulgaricus and Streptococcus thermophilus) are producers of lactase too. (González S, Martínez A, Puesta en común IL, Cap3, FEAD 2017)
4. The consistency or viscosity of this type of product slows down its digestion, delaying gastric emptying and modulating intestinal motility, causing the lactose to be released more slowly in the duodenum and to be maintained in the small intestine for longer. This slowing down will cause the lactose to be present for longer in the intestine in contact with residual lactase, optimising its action. (Labayen I, Forga L, González A, et al. 2001)

-
16If I don't want to reject dairy, what are my alternatives?
If you don’t want to reject the taste and nutritional properties of cow’s milk, in recent years there has been availability of milk brands on the market where the lactose has been eliminated or previously partially hydrolysed called ‘low in lactose’ or totally hydrolysed called ‘lactose-free’. This range has been complemented with dairy-derived products such as different varieties of cheese (gouda, emmental, etc.), yoghurt, flavoured milkshakes, cream etc.
You can also find lactase supplements in the pharmacy in the form of tablets/capsules/drops that will allow you to consume dairy products. These are recommended for sporadic use if eating outside the home and you’re not sure whether the dishes contain lactose or not, when attending a business dinner, a celebration etc. These tablets provide the organism with the lactase that we need to break down the lactose in a specific meal, so you should take it each time you eat because the effect is momentary. The main issue is finding the right dose, as this will always depend on various factors (question 4) but particularly on the relationship between your level of intestinal lactase and the amount of lactose ingested.
-
17Can it be considered to be an illness?
Taking into consideration that approximately 2/3 of the global population, i.e. the majority, suffers from this deficiency, we cannot consider it to be an illness, but rather an inability to digest milk sugar.
-
18What type of milk is most consumed in the world?
The most produced and consumed type of milk in the world is cow’s milk, but in second position -sure that you did not imagine it- is buffalo milk.

-
19What is milk and what isn't?
The definition of milk is ‘the secretion from female mammals with the purpose of satisfying the nutritional requirements of the newborn during their first years of life’.
In the regulations of our country, ‘milk’ can only be used to refer to ‘cow’s milk’. To refer to milk from other animals, the name of the species must be specifically designated: ‘sheep milk’, ‘goat milk’, ‘buffalo milk’, ‘maternal milk’.
Plant-based drinks (soy, rice, hazelnut, oat, tiger nut, etc.) can never be advertised as milk, only as plant-based drinks. With the exception of ‘almond milk’ due to its traditional and historic denomination in our country. In other countries such as France, this is true for ‘coconut milk’.
For milk to continue to be called ‘milk’, only certain industrial treatments are authorised:
· Modification of fats.
· Addition of vitamins and minerals.
· Addition of lactase.Any other treatment will not permit the denomination of ‘milk’ and must be called ‘dairy product’ or ‘dairy drink’.
-
20How much lactose is there in milk?
Lactose is the second component of milk after water. The percentage of lactose present, as well as the other components, will vary depending on the type of cow, how it was fed, the chemical treatment it was subjected to, etc. In the composition we must distinguish between:
· Water 87%
· Dry extract (sugars, fats and proteins) 11%
· Vitamins and minerals 2%

-
21How are lactose-free products prepared?
There are two technological methods used by the food industry to eliminate lactose from dairy products:
1. Hydrolysis of lactose through the addition of lactase (A type of microbial B-galactosidase derived from micro-organisms such as Kluyveromyces lactis, Kluyveromyces fragilis or, to a lesser extent, Aspergillus oryzae). If this method is used, it can be called milk.
2. Partial elimination of lactose through physical methods such as ultrafiltration or chromatography. This method is normally used in combination with hydrolysis. If this method is used, it cannot be called milk.
-
22Why is lactose-free milk sweeter?
Lactose-free milk (when it is prepared through hydrolysis) is sweeter than ordinary milk because during the hydrolysis process the lactose is broken down into two simple sugars (glucose and galactose) that together are sweeter (87) than lactose itself (22). On the table is a comparison of the relative sweetness of different sugars compared with the 100% value of sacarose (ordinary white sugar).
If the lactose-free milk has been prepared through physical means where part of the lactose is eliminated through physical means, the milk will be practically just as sweet.

-
23What information is on the product labeling?
On the labeling of any food product we will find:
Mandatory information
· Basic information of the product: Denomination, weight, origin, expiration, etc.· Nutritional table (p / 100g): Energy / Kcal, Hydrates (sugars), Fats (saturated), Proteins, Salt.
· List of ingredients: Ingredients ordered according to the amount present in the product.
Interpretable information
· EPA Precautionary labeling of allergens: Although it is contemplated in R1169 / 2011 (art. 36.3) there is still no regulatory development that defines how to declare it. In this sense, AESAN considers that this type of warnings “may contain + allergen” should only be used in cases where the manufacturer cannot guarantee after applying its internal control systems (safety, hygiene and HACCP) the absence of this allergen in the final product. And in no case should it be used by the manufacturer as an “easy” resource for not complying with the food safety and control procedures required of it.Voluntary information
Only those declarations that are authorized and the product meet the required conditions can be used in the nutritional and health claims.· Declaration of nutritional properties: no sugar, omega-3 source, low in salt, fiber source, vitamin C source, calcium source, etc.
· Declaration of healthy properties: Relating to the growth and health of children, reducing the risk of certain diseases, vitamin C contributes to the functioning of the immune system, etc.
· Differentiated product attributes: Mentions or stamps such as Eco, Km0, Recyclable, homemade, traditional, vegan, kosher, gluten-free, lactose-free, halal, palm oil-free, BPA-free, etc. Depending on the attribute, there may or may not be a usage regulation.

-
24How do I know I can consume a product reading the label?
When an IL reads the labeling of a packaged product, it finds three types of information:
· List of ingredients (OBLIGATORY)
In the list of ingredients, the presence of any of the 14 main allergens -including milk, and derivatives, including lactose- must be highlighted. If Milk, derivatives or lactose appear in the list of ingredients.· Precautionary information (VOLUNTARY/OBLIGATORY)
The manufacturer includes precautions mentions of the type “may contain traces of milk”, “there may be a cross contamination of milk to be made in a plant where dairy is worked”, etc. stating that it cannot guarantee the absence of milk due to possible cross contamination.· Attribute information (VOLUNTARY)
The manufacturer includes differentiated product attributes in form of text or logos like “no lactose”, “lactosefree product”, etc. manifestly expressing that it guarantees the absence of milk/lactose in the final product.In the following graph you can see our consume recommendation when the IL faces this peculiarities of labeling a packaged product.

-
25Nutritional information is useful to know if a product is lactose-free?
No. The nutritional information is not intended to be useful to inform about the presence of allergens or substances that cause food intolerances, such as lactose, and does not serve to conclude that a product without carbohydrates and sugars, is a “lactose-free” product. We explain why.
The nutritional information of any food product can be prepared by the manufacturer from three sources:
1.The analysis of the final product carried out by the manufacturer in a laboratory.
2.The calculation made by the manufacturer from the known / effective average values of all the ingredients used (for example, from the data of the ingredients provided by their own suppliers).
3.The calculation from established and accepted data (Bibliography in tables of mean content of nutritional values of different foods).Therefore, the actual amount of a nutrient in a product may vary compared to the declared value on the label, due to factors such as:
-The accuracy of the analysis.
-The indirect source from which the values were obtained (calculated by recipe or bibliography).
-The variability of raw materials.
-The effect of transformation on raw materials.
-The stability of the nutrients.
-The storage conditions and time.Even so, the nutrient content of the food may not differ substantially from the declared / labeled values to the extent that such differences could mislead the consumer. For this purpose, minimum and maximum accepted tolerances / deviations have been established for the nutritional values that manufacturers must comply with, you can consult them in the following Guidance Document of the European Commission.
Table 4 of this guide document establishes the Rounding Rules for nutritional information on the labeling of nutritional properties of food products, and specifically for specific sugars, “if no detectable quantities are present or the concentration is ≤ 0.5 g per 100g or ml, the rounding rule is that “0g” or “0.5g” can be declared”.
In addition, and regarding the nutritional declarations that can be made on food, they are exclusively those established in the annex to EU Regulation 1924/2006. This annex includes the declaration “WITHOUT SUGARS” establishing the following conditions of use: “It can only be declared that a food does not contain sugars, as well as any other declaration that may have the same meaning for the consumer, if the product does not contain more than 0.5 g of sugars per 100 g or 100 ml. “
In summary. The Nutritional Information and Nutritional Declarations on the content of Carbohydrates / Sugars in a food product are not information to be followed to consider a lactose-free product.

-
26Can I take a medicine that contains lactose?
Lactose is incorporated as an excipient in 40% of currently authorized medicines (source AEMPS). This can be a problem for some patients with very low tolerance levels, and makes it difficult for the doctor to prescribe an appropriate medication in these cases.
So, can I consume a medicine with lactose as an excipient? It will depend on:
A. The lactose intolerance degree of each person.
B. The amount of lactose ingested with the medication. Quantity that will result from the formula (B1 x B2) + B3.B1. The amount of lactose contained in a dose (pill, capsule, dragee) of the medicine.
B2. The amount of total doses taken.
B3. In the case of being a polymedicated person, the amount of lactose ingested by other medications. -
27How do I know if a medicine contains lactose and in what quantity?
You have two ways to know if a medicine contains lactose:
Medication leaflet
To find out if a drug contains lactose, you can read directly from its leaflet (in sections 2 and 6).Web CIMA-AEMPS
To find out if a drug contains lactose and also the exact amount that a dose contains (Mg), you can perform a search for the drug on the CIMA·AEMPS. There you will be able to consult the same leaflet of the medicine in digital format and also in the Technical Data Sheet of the medicine the exact amount of lactose in Mg (section 2) so that you can calculate how much lactose you are consuming each day with the medication.
-
28If I stop consuming lactose, will my intestine stop producing lactase and will I be even more intolerant?
This is a frequently asked question, and there is no scientific agreement on it.
There are studies that:
-They claim that consuming lactose or not consuming lactose influences lactase production levels in our intestines. That is, if you take lactose, more lactase is produced and if you reduce the intake of lactose, less lactase is produced.
-Other studies affirm that the amount of lactase that we have in our intestines -at different stages of our life- is genetically defined. According to these studies, whether or not consuming lactose will not cause us to produce more or less lactase in our intestines.

