-
01
Exhaled breath test

This is currently the most frequently used method to measure poor digestion of lactose, although it has limitations for application when used on children aged under 4-5 years. The patient is given a solution with lactose (25-50g of lactose in 200-400ml of water) and after intervals of 15 minutes they are asked to blow into hermetic bags/test instrument/test tubes where samples are collected. When the undigested sugars are transported to the large intestine, the bacteria present there uses them as food and create hydrogen as a waste product. The hydrogen is absorbed by the blood flow and expelled through respiration. The hydrogen detected in the respiration indicates that the sugar has entered the large intestine, not correctly absorbed in the small intestine. There must be increased hydrogen H2 in the respiration after ingesting the lactose of over 20 ppm to indicate deficient digestion. This test also assesses the presence of Methane CH4 in order to avoid possible false negatives (particularly in people whose intestinal flora does not produce hydrogen as a reaction), and in this case the increase detected after the ingestion of lactose must be above 12ppm. Sample sensitivity results Isomed Pharma
-
02
Blood test for lactose overload/tolerance

This is another method to measure digestion of lactose but is considered to be less reliable than the former. In this method, first blood is taken from the patient in order to learn their basal blood sugar (initial or reference level of glucose in blood). Then, like in the hydrogen test, they are given 100 grams of lactose in a solution with water. Then, after 60 and 120 minutes, new blood samples are taken. If there is no release of glucose, due to lack of lactase action that should be in the intestine, there is no absorption of glucose to the blood flow through the intestinal wall and therefore the level of glucose in the blood does not increase. Therefore, it cannot be said that there is an poor digestion/absorption of lactose. It can be said that there is poor digestion of lactose if the blood sugar level after taking the lactose does not go above 20 mg/dl with regards to the basal (initial) value. Examples of positive and negative results of sensitivity among patients Sample results patient sensitivity
-
03
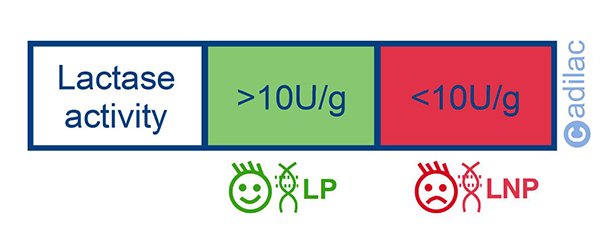
Biopsy of small intestine

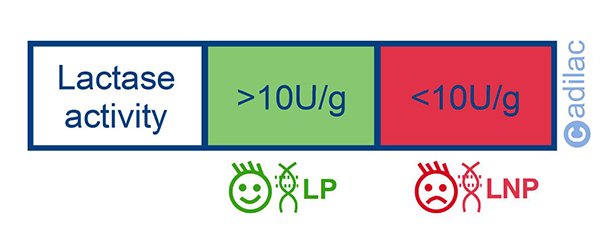
This is a method that permits measurement of the LNP. It is an invasive method because obtaining the samples for posterior analysis takes place through the performance of an endoscopy or EGD (eophagogastroduodenoscopy) of the upper gastrointestinal tract (duodenum or jejunum). The test is normally carried out with full sedation of the patient. A flexible fibre optic tube (endoscopy) is inserted to the patient through the nose or mouth towards the upper gastrointestinal tract. The samples of tissue obtained during the endoscopy are sent to the laboratory for examination and the lactase activity of the tissues/mucosa extracted is assessed. Lactase activity below 10U/g of protein is considered to be related to LNP or lactase deficiency.
-
04
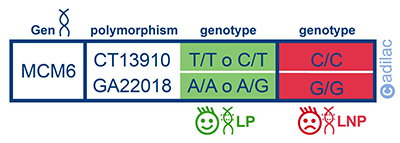
Genetic test

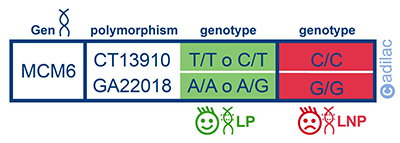
Primary lactase deficiency (LNP) has a genetic determination. Recent studies in this sense establish that lactase activity is associated to the presence of two polymorphisms identified in the gene MCM6. This method consists of extracting and amplifying the DNA of a sample (the patient’s blood or saliva), continuing with a protocol of strip hybridisation in order to detect the presence of certain genotypes: Individuals who are carriers of the CC genotype of the polymorphism C/T 13910 and the GG genotype of the polymorphism G/A 22018 present primary hypolactasia. The final practical result is a series of coloured bands on a strip that are interpreted with the help of a template. The result provides the specialist with information on the genetic predisposition to suffering from primary lactase deficiency or LNP. Examples of sensitivity results by Operon
-
05
Gaxilose test

This recent method permits measurement of lactose digestion. The diagnosis is based on the oral administration of a low dose of Gaxilose (chemical name 4 galactose-xylose), a synthetic disaccharide similar to lactose that is hydrolysed by intestinal lactase in galactose and xylose, with the latter reaching the urine. The amount of xylose detected in urine is proportional to the level of intestinal lactase activity, therefore this figure can be used to measure the poor digestion of lactose and to help with the diagnosis of the acquired or primary hypolactasia. If the quantity of xylose excreted in all of the urine accumulated during the five previous hours is less than 19.18 mg, the patient has hypolactasia. It is a direct measurement of the lactase activity with a very low dose of sugar that does not usually cause discomfort during the test. Sample sensitivity results Venter Pharma
-
06
Other methods

Faecal tests pH determination: For nursing infants with a suspicion of lactose intolerance, samples of fresh faeces can be obtained through a rectal examination, and with the most liquid part carry out the pH determination through reactive strips, discriminating from half to half point to check acidity, and the determination of the presence of reducers and/or glucose through Clinitest tablets or Clinistix reactive strips.